The concept of Natural Power Antibiotic Resistance: What is it, and how are we involved?
Antibiotic resistance (ABR) is the ability of bacteria (or other microbes) to resist the effects of an antibiotic that would normally kill them or stop their growth. In other words, the bacteria survive and continue to multiply despite the presence of antibiotics that were once effective against them. According to Dr Roelof Coetzee, a South African doctor currently doing research on ABR in Sweden,1,3 million people died in 2019 due to ABR. This happens through natural selection, co- selection and genetic changes, often accelerated by misuse or overuse of antibiotics in humans, animals, agriculture and global travel and trade.
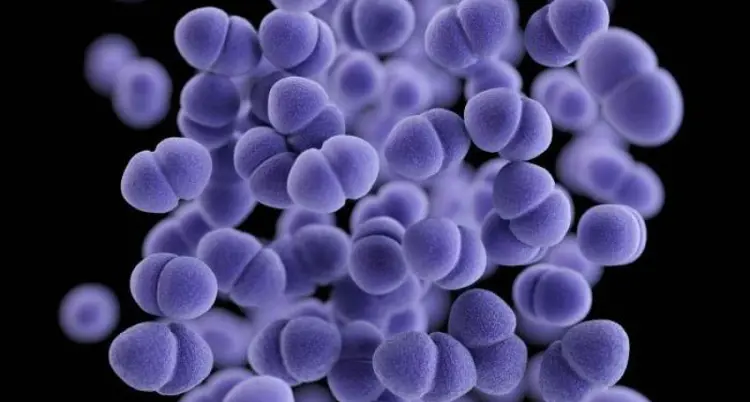
Selection: When a bacterial infection is treated with an antibiotic, there are always a few of these bacteria that are resistant to the antibiotic. This is probably because antibiotics are produced by other microbes like fungi and other bacteria, which occur naturally and to which the problematic bacteria have been exposed. They will survive, and when they grow again after treatment, the % of ABR bacteria is larger, and the survival rate increases. The more often antibiotics are used, the faster the ABR increases.
This is often accelerated by people not completing an antibiotic course, or sharing of antibiotics, or when antibiotics are used for flu symptoms that are viral and not bacterial.
Genetic changes: Bacteria can exchange DNA with each other. A resistant, non-dangerous bacteria can exchange DNA and cause, for example, a non-resistant bacteria to become resistant.
Co-Selection: Research teams working on ABR have discovered that some bacteria have shown resistance against antibiotics to which they have never been exposed. This resistance was developed by exposure to rare earth metals. These rare earth metals are being mined increasingly to supply mainly the green technologies like wind turbines, car (EV) batteries, cell phones, etc.
Mining of these rare earth metals causes a release into the environment, resulting in increased ABR amongst bacteria. This happens especially around mine areas where most of the pollution around mines, which yields metals.
The misuse of antibiotics: All the above-mentioned factors are augmented by the misuse of antibiotics by humans, such as irresponsible prescription of antibiotics, non-completion of an antibiotic course, using old, unused antibiotics, sharing of antibiotics, and uncontrolled procurement of antibiotics over the counter (OTC). Antibiotics are often prescribed for viral infections like the flu, where it has no impact – they only work on bacterial infections.
A study led by researchers at the Oxford University Clinical Research Unit in Vietnam investigated antibiotic access and OTC use in six countries. The study found that (cidrap.umn.edu+1theguardian.com+1):
• Vietnam: 55.2% of antibiotics were obtained without a prescription.
• Bangladesh: 45.7%
• Ghana: 36.1%
• Mozambique: 8%
• Thailand: 3.9%
• South Africa: 1.2%
This brings us to the last driver, which is international travel and trade. Although SA has a relatively low access to OTC (1,2%), international travel and trade can spread ABR bacteria throughout the world.
Where do we use antibiotics in animal production, and how important is the contribution of those usages to ABR?
There are a few Antibiotics that are generally used in animal production to maintain health and increase production.
• They can be classified as prophylactic antibiotics (feed additives like ionophores) and
• Antibiotic therapy refers to the use of antibiotics to treat infections caused by bacteria.
• If the treatment is started before the exact bacteria are identified, it's called empiric antibiotic therapy.
• Once the specific bacteria are known and the antibiotic is chosen accordingly, it's called targeted (or definitive) antibiotic therapy.
• The most common problem is that much of the antibiotic therapy is applied in a blanket approach, and not really in a targeted approach.
What are Ionophores?
• Ionophores are antibiotics used exclusively in animals, not in human medicine.
• They help control infections like coccidiosis in poultry and ruminants and improve feed efficiency. We saw in the previous article that cattle numbers reduced, but meat yield increased, due to increased production related to the use of ionophores.
• Examples: Monensin, Lasalocid, Salinomycin.
Do Ionophores Contribute to Antibiotic Resistance in Humans?
- Direct contribution is unlikely:
- Since ionophores are not used in human medicine, there is no direct selection pressure for resistance to human-use antibiotics. (not MIA)
- Ionophore resistance genes are not known to be shared with clinically relevant antibiotics (as of current research).
- Indirect effects are possible:
- Ionophores can still alter the gut microbiota in animals, which might:
- Increase horizontal gene transfer (HGT) among bacteria.
- Select for multidrug resistance plasmids if they're co-located with ionophore resistance genes (though this is rare).
- Ionophores can still alter the gut microbiota in animals, which might:
- Use of any antimicrobial may contribute to a general resistance-promoting environment in animal gut flora or manure that can reach the environment or food chain.
This is where the classification of antibiotics becomes important. 2 bodies have classified antibiotics in terms of MIA (Medically Important Antibiotics). They are the WHO (World Health Organisation) and EMA (European Medicines Agency). The EMA categorization classifies antibiotics into four categories (A–D): Ionophores used in animal feed fall in the D category.
|
Category |
Examples |
Comments |
|
A (Avoid) |
Rifampin, Linezolid, Carbapenems |
Last-resort drugs for humans |
|
B (Restrict) |
Fluoroquinolones, 3rd/4th-gen cephalosporins, Col- istin |
Use only under strict conditions |
|
C (Caution) |
Macrolides, Aminoglycosides, Tetracyclines |
Use when Category D drugs are not effective |
|
D (Prudence) |
Penicillin, Sulfonamides, Ionophores |
Common in veterinary medicine and feed, lower AMR risk |
Table 1 . EMA Categorization of antibiotics.
What is important for animal production can be found in The Codex Alimentarius
The Codex Alimentarius Commission has developed guidelines on the use of antimicrobials in food-producing animals, including AMGPs. For those interested, the details are too much to fit in this article; they can be viewed at the following address:
• Codex Alimentarius Commission Website: www.fao.org/fao-who-codexalimentarius
Summary
If we look at all the statistics on the low levels at which OTC antibiotics are used for therapy in SA (1,2%), and the fact that we make use of ionophores, which are not an MIA antibiotic and not used in humans, we wonder why all the fuzz? The reality is that with all the other environmental effects and impacts from, for example, rare earth metal pollution by mines, international travel and trade, unsupervised use of antibiotics, etc, we might be making a contribution to co-selection and genetic mutation of bacteria that are resistant to antibiotics.
Of much more importance is the public perception of the use of antibiotics in animal feed and the impact it could have on AMR. If the consumers of our products (informed or not) are resisting buying the end product due to the possible impact on AMR, we need to act. Fortunately, there are alternatives which can be used that yield similar (and even better) results. This encompasses a total management approach, which will be discussed in the following article on the Natural Power concept of De Heus.
For more information on the concept of Natural Power, please contact your De Heus technical advisor - https:// www.deheus.co.za/meet-our-team/.
